The Muscle–Longevity Connection: The Science of Preserving Muscle with Age
Muscle predicts longevity better than body size.
Muscle mass and strength are stronger predictors of survival than BMI in older adults. Something as simple as grip strength can forecast disability, hospitalization, and lifespan more accurately than weight or body fat.
Sarcopenia is driven by multiple aging pathways.
Muscle decline isn’t just disuse — it stems from mitochondrial dysfunction, nerve-muscle disconnection, hormonal shifts, chronic inflammation, anabolic resistance, satellite cell loss, and overactive mTORC1. These overlapping mechanisms explain why simple fixes have failed.
Strength training is the most effective intervention.
Resistance training consistently improves grip strength, gait speed, balance, and quality of life. Multicomponent programs that combine resistance, aerobic, and balance training yield the biggest benefits for functional independence in older adults.
Protein intake is a critical partner to exercise.
Older adults require 1.2–1.5 g of protein per kilogram of body weight daily — far above the standard RDA. Leucine-rich proteins (around 3 g per meal) help overcome anabolic resistance, making dietary quality as important as quantity.
Muscle acts as medicine for the whole body.
Far beyond strength, muscle functions as an endocrine organ. Exercise-induced myokines improve metabolism, reduce inflammation, and protect the brain and immune system, making muscle one of the body’s most powerful anti-aging tissues.
It’s never too late to build strength.
Even elderly adults who begin resistance training for the first time experience meaningful improvements in strength, balance, and independence. Age slows the rate of growth, but the capacity to adapt never disappears.
Sarcopenia and Strength
Sarcopenia is the inevitable age-related decline in muscle mass (Figure 1) and is a major contributor to falls, hospitalization, and diminished quality of life in older adults. Unlike some age-associated conditions, however, sarcopenia has a powerful antidote that’s both accessible and scientifically supported: exercise and nutrition – specifically dietary protein. While pharmacological treatments remain underwhelming, decades of clinical research now converge on a clear conclusion: strategic combinations of resistance training and high-quality protein intake are among the most effective interventions available. With sarcopenia affecting over 50 million people globally, a number expected to quadruple in the coming decades, it’s paramount that we prioritize prevention and treatment strategies that are backed by data.
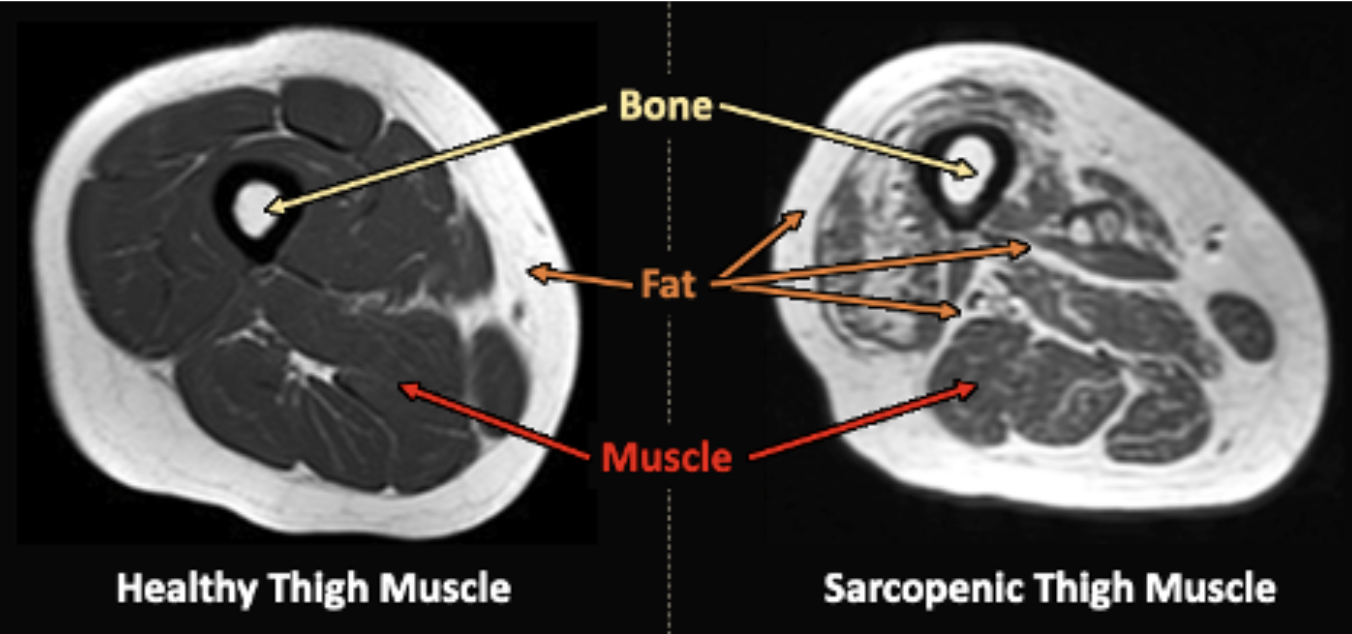
Figure 1. MRI cross-sections of a relatively young and healthy thigh muscle (left) and an older, sarcopenic thigh muscle (right). Note the greater infiltration of fat tissue throughout the muscle in the sarcopenic thigh. Adapted from “Ultrasound and magnetic resonance imaging as diagnostic tools for sarcopenia in immune-mediated rheumatic diseases (IMDRs),” by F. Salaffi et al., 2022, La Radiologia Medica, 127: 1284 [1].
When looking at Figure 1, it’s easy to understand why sarcopenia has such a negative impact on our quality of life. If we have less muscle, we are weaker and less capable of moving our bodies, and, therefore, less capable of independent living. Carrying groceries, placing our suitcase in the overhead bin on a plane, and even standing upright become more challenging with decreasing strength. This can have a compounding effect on osteoporosis, in that the more our muscles wither, the more our bones degrade, too. In fact, the dual decline of muscle health and bone health with aging, or sarcopenia and osteoporosis, respectively, has been called “osteosarcopenia” when both meet minimum clinical criteria for diagnosis [2]. A vicious cycle can develop for an older adult suffering from sarcopenia that fosters and/or accelerates osteoporosis (Figure 2).
Additionally, muscle plays a critical metabolic role in the body, and having less of it can exacerbate certain metabolic conditions. In 2019, the annual health care costs resulting from sarcopenia in the United States were estimated to be $40.4 billion [3], which is only expected to increase drastically with a growing geriatric population. Adoption of effective interventions to combat sarcopenia has become a race against both the individual’s and the world’s clocks.
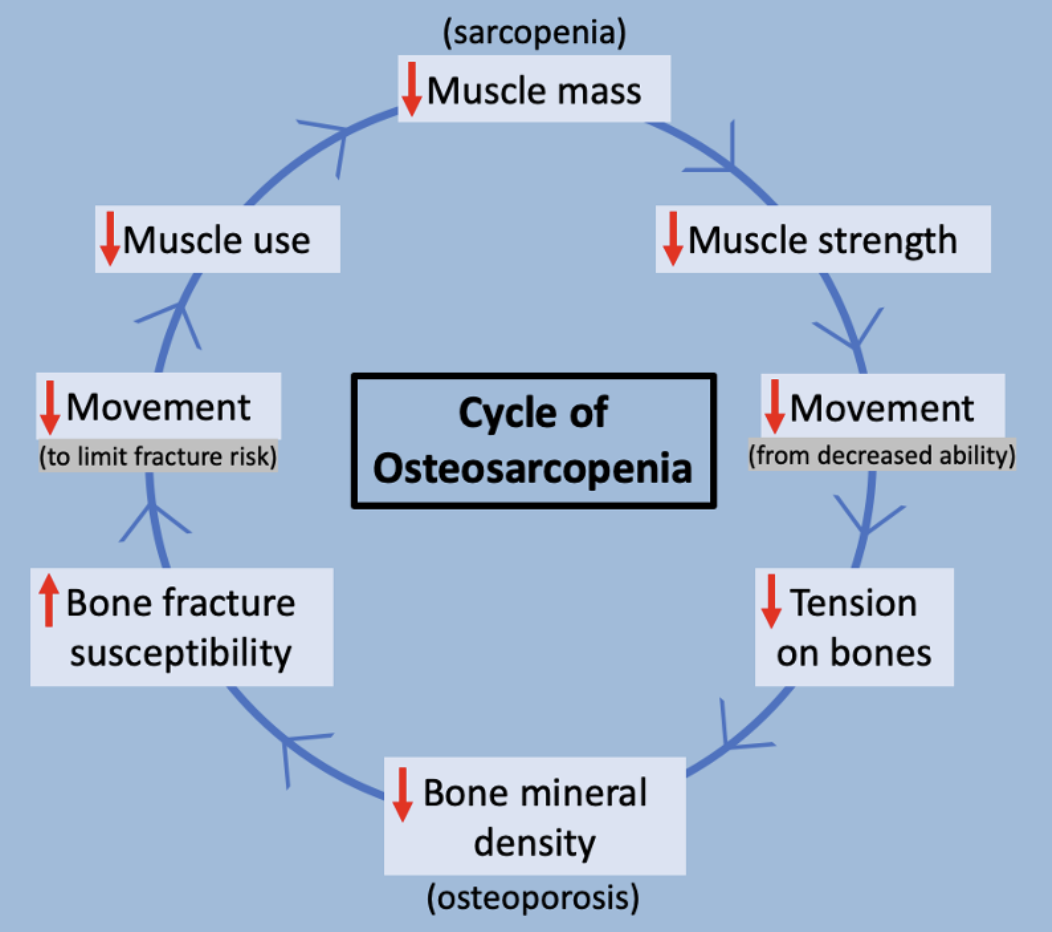
Figure 2. A cycle of osteosarcopenia (concurrent osteoporosis and sarcopenia) that older adults can experience.
Sarcopenia Quick Facts:
- Sarcopenia is a progressive skeletal muscle disorder common in aging adults, associated with higher risks of disability, falls, hospitalizations, and mortality.
- The prevalence of sarcopenia increases from 5–13% in adults aged 60–70 to 11–50% in those over 80 [4].
- No pharmacological treatment for sarcopenia has been FDA-approved, making non-drug interventions such as resistance exercise and protein intake first-line therapies.
- Sarcopenia is also a common complication in patients with chronic diseases such as cancer, obesity, and diabetes, and its presence in these populations worsens outcomes and increases healthcare costs.
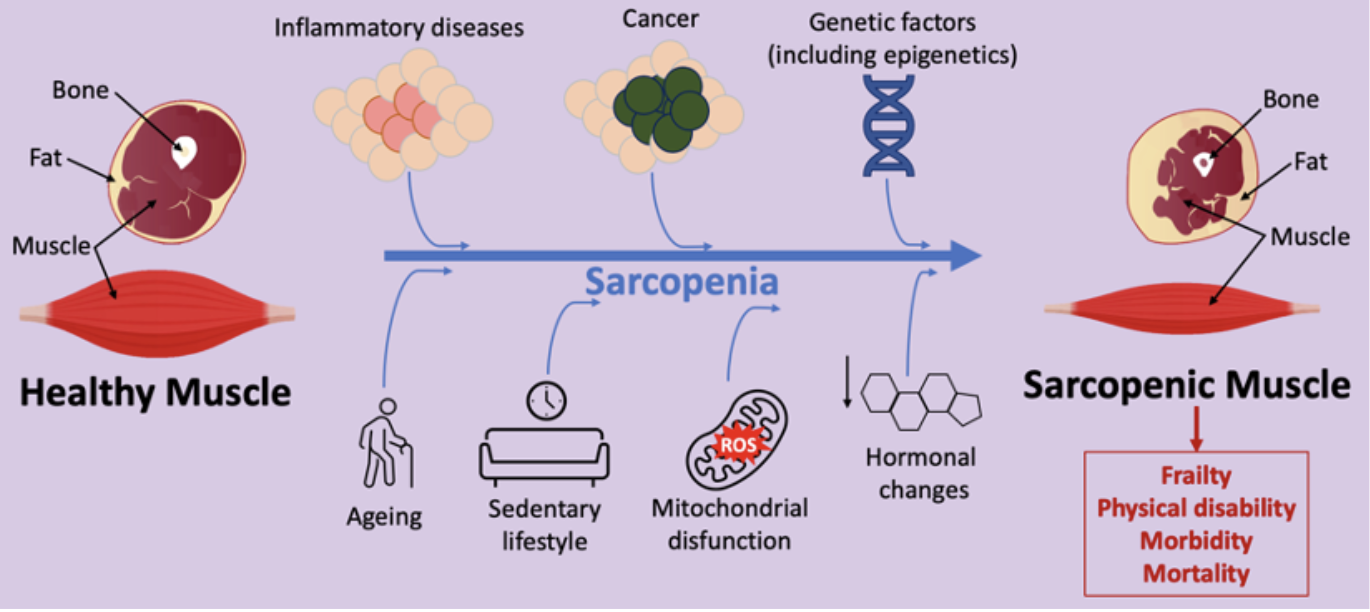
Figure 3. Schematic representation of major factors contributing to sarcopenia and effects on human health identified by Nasso et al. (2024) [5].
Mechanisms of Sarcopenia: Why Muscles Shrink with Age
Sarcopenia may look like a simple case of “muscle loss,” but under the surface, multiple biological systems gradually erode the body’s ability to maintain muscle mass and function. Last week we discussed one particular mechanism — the mTOR insensitivity that develops with aging and contributes to anabolic resistance. But like most forms of age-related tissue dysfunction, sarcopenia is driven by a network of interwoven pathways that can each go awry in different ways. Understanding these mechanisms highlights why interventions such as exercise and protein are so effective — and why pharmacological approaches have, so far, struggled to match them.
1. Mitochondrial Dysfunction
Aging muscle fibers experience a decline in mitochondrial number and efficiency. With less capacity to generate ATP, muscles lose the energy needed for contraction, repair, and regeneration. Mitochondrial dysfunction also increases reactive oxygen species, which further damage muscle proteins and DNA [16, 17].
2. Neuromuscular Junction (NMJ) DegradationThe communication between nerves and muscle fibers weakens with age. Motor neurons retract from some fibers altogether, leading to “denervation” and fiber atrophy. This explains why sarcopenia is not just about mass but also about reduced coordination and strength [18].
3. Hormonal Shifts
Declining levels of anabolic hormones such as testosterone, estrogen, growth hormone, and IGF-1 reduce the body’s ability to stimulate muscle protein synthesis. At the same time, increased activity of catabolic pathways (such as myostatin signaling) promotes muscle breakdown [19, 20].
4. Chronic Inflammation (“Inflammaging”)
Even in the absence of overt disease, older adults often experience elevated pro-inflammatory cytokines (IL-6, TNF-α, CRP). This “smoldering” inflammation accelerates muscle breakdown, blunts anabolic signaling, and contributes to insulin resistance [21, 22].
5. Anabolic Resistance
Older muscle becomes less responsive to dietary protein and exercise stimuli, a phenomenon known as anabolic resistance. This is why older adults often need higher protein intakes and more consistent training to achieve the same gains as younger individuals [23].
6. Satellite Cell Dysfunction
Satellite cells are muscle stem cells responsible for repair and regeneration. With age, their number and activity decline, reducing the capacity to rebuild muscle after injury or training [24].
7. mTOR Hyperactivity & Impaired Autophagy
Recent research shows that in aging muscle, the mTORC1 pathway can become chronically “on.” While mTORC1 is essential for muscle growth, this persistent activation paradoxically contributes to anabolic resistance, suppresses autophagy (the cell’s repair and cleanup system), and fosters the accumulation of damaged proteins and organelles. The result is diminished muscle quality and resilience. As discussed in our recent article on rapamycin and muscle preservation, intermittent modulation of mTORC1 — for example with low-dose rapamycin — may help restore balance between anabolic signals and cellular repair, offering a novel therapeutic angle.
Together, these processes create a “perfect storm” in which muscle mass declines, strength wanes, and function deteriorates. Importantly, resistance training and adequate protein intake target many of these mechanisms simultaneously — improving mitochondrial health, re-sensitizing muscle to anabolic signals, and reactivating satellite cells.
The Longevity Connection: Why Muscle Is Medicine
Muscle is often thought of as a tool for movement, but mounting evidence shows it acts as a powerful biomarker — and even a driver — of long-term health and survival. In fact, muscle mass and strength predict longevity more reliably than traditional measures like body mass index (BMI). Older adults with greater muscle mass and grip strength consistently live longer and enjoy better functional independence than those with similar BMI but lower muscle reserves [25].
Sarcopenia also correlates with faster progression on biological aging clocks. Declines in muscle mass and function track closely with other hallmarks of aging, from mitochondrial dysfunction to immune decline. In this sense, sarcopenia is not just a symptom of aging — it is one of its most visible accelerators.
Beyond survival, muscle serves as a metabolic buffer. By taking up and storing glucose, skeletal muscle protects against insulin resistance, type 2 diabetes, and the metabolic syndrome [26]. This helps explain why individuals who maintain muscle into later life show lower risks of cardiovascular disease and better overall metabolic resilience.
Emerging evidence suggests muscle may even extend its protective effects to the brain and immune system. Regular resistance training and preserved muscle mass are associated with reduced dementia risk, greater cognitive performance, and improved immune competence [27, 28]. Through exercise-induced myokines and other signaling molecules, muscle communicates with organs as diverse as the liver, adipose tissue, and brain — influencing systemic inflammation, energy balance, and neuroplasticity.
Taken together, these findings reinforce that muscle is not only a tissue of movement, but also a tissue of medicine. Protecting it through exercise and nutrition is one of the most potent ways we can intervene on aging itself.
Which Training Methods Protect Muscle as We Age?
In a 2023 network meta-analysis of 42 randomized controlled trials with a combined 3,728 older adults (age ≥60 years) with sarcopenia, researchers compared the effectiveness of different types of exercise and nutrition interventions for treating sarcopenia [4]. The results were promising:
Resistance Training Alone:
- Consistently improved handgrip strength (mean difference [MD]: 2.69 kg), which is a simple test highly correlated with total body strength, bone mineral density, and even mortality in older adults [6].
- Showed moderate evidence for improving physical function on standardized tests of gait speed (natural walking speed), chair-stand (time to stand up and sit down for five repetitions), and timed-up-and-go (time to stand and walk a certain distance), all of which are relevant measures of physical ability for older adults.
- Had the largest effect of any single type of exercise assessed for improving quality of life.
Key Takeaway: Resistance training alone improves performance on direct tests of strength and can improve performance on other tests where strength is a critical component. Also, resistance training will help counter the impact more than any other type of exercise.
Resistance + Aerobic + Balance Training:
- Associated with the greatest improvements in quality of life, with high-certainty evidence showing large standardized mean differences (range of 0.68-1.11) compared to “usual care” (varies by study, but often some nutritional supplementation). What this means is that intervention groups practicing resistance, aerobic, and balance training improved quality of life metrics by 0.68 to 1.11 standard deviations greater compared to “usual care” control groups.
Key Takeaway: training multiple facets of physical performance – specifically strength, cardiovascular endurance, and balance – should have the biggest benefit on measures of overall quality of life.
Resistance Training + Balance Training + Nutrition:
- Added nutritional support produced clinically meaningful increases in strength (mean difference: 4.19 kg) and other tests of physical function (e.g., +0.16 m/s in natural walking speed).
Key Takeaway: This was the most effective for improving overall physical function and handgrip strength. Resistance training with adequate protein intake best supports strength gains. Adding balance training enables individuals to effectively apply their strength gains to broader physical function tests, theoretically through improved coordination and control of body weight.
These findings validate existing clinical recommendations that prioritize multicomponent physical activity – especially resistance training – alongside nutritional support as the foundation for sarcopenia management.
Protein Intake: Optimizing Muscle Protein Synthesis Over Degradation
In parallel, a 2024 review by Nasso et al. [5] analyzed the impact of dietary protein quality and quantity on muscle preservation in aging populations. Protein plays a vital role in stimulating muscle protein synthesis, especially when paired with exercise. But not all proteins are created equal, and both the amount and type of protein can dramatically influence outcomes for older adults.
- Study Findings: Older adults often require 1.2–1.5 g of protein per kg of body weight per day to counteract anabolic resistance and prevent muscle loss, which is significantly higher than the recommended dietary allowance of 0.8 g/kg/day, and echoes the findings of a recent systematic review and meta-analysis [7]. This higher requirement reflects the reduced sensitivity of aging muscle to dietary protein.
- Essential amino acids – especially leucine [8], a branched-chain amino acid (BCAA) – are critical triggers for muscle protein synthesis (muscle growth). About 3 g of leucine in a serving of protein maximizes muscle protein synthesis in older adult males [9]. Insufficient leucine intake was consistently associated with blunted muscle response, even when total protein intake was adequate. Insufficient leucine intake was consistently associated with blunted muscle response, even when total protein intake was adequate.
- Animal proteins (e.g., eggs, dairy, meat) tend to have higher leucine content and better digestibility than plant-based proteins, which was even more recently supported by Matthews et al. (2025) [10]. However, a well-planned plant-based diet with sufficient leucine (from peanuts, soybeans, lentils, etc.) can still support muscle maintenance and growth.
- Combining dietary protein with resistance training amplifies muscle-building effects, even more than either intervention alone.
Older adults often require 1.2–1.5 g of protein per kg of body weight per day to counteract anabolic resistance and prevent muscle loss, which is significantly higher than the recommended dietary allowance of 0.8 g/kg/day, and echoes the findings of a recent systematic review and meta-analysis. This higher requirement reflects the reduced sensitivity of aging muscle to dietary protein.
Plant-Based Protein or Animal-Based?
One randomized trial cited in Nasso et. al’s 2024 review showed that leucine supplementation (or its metabolite HMB) significantly reduced muscle breakdown in elderly participants [11]. Other studies suggest plant-based diets may reduce inflammation and oxidative stress, potentially offering additional benefits in age-related muscle decline by supporting mitochondrial health [12]. Taken together, these findings suggest that while animal-based protein sources make adequate leucine intake easier to achieve, plant-based protein sources may better support an older individual’s broader health goals if reduced inflammation is a priority. A combination of plant- and animal-based proteins likely checks the most health boxes for most people.
Health Benefits Beyond Strength & Function: Muscle as an Endocrine Organ
The benefits of physical activity are not limited to muscle strength and coordination. Exercise-induced myokines, such as IL-6, IGF-1, irisin, and BDNF, serve as molecular messengers that influence whole-body metabolism, reduce inflammation, and promote neuroplasticity [5]. This explains why physical activity improves not only muscle strength and function but also cognitive function, metabolic health, and resilience to chronic diseases. Conversely, inactivity reduces circulating levels of these protective molecules, compounding the progression of sarcopenia and related disorders. So even if the benefits of strength training aren’t enough motivation to get started, it can help to remember the consequences associated with a sedentary lifestyle; it’s about achieving something good as much as it is about avoiding something bad.
Practical Takeaways & How To Implement
Exercise: The National Strength and Conditioning Association’s position statement on resistance training for older adults recommends 2–3 sets of 1–2 multijoint exercises per major muscle group at exercise intensities of 70–85% of an individual’s 1-repetition maximum performed 2–3 times per week [13]. This can be a helpful framework, but the average older adult is not likely to perform 1-repetition maximum testing on their exercises, so we need a simpler approach to get started:
- Frequency: at least 2 times per week, separated by a few days of rest, is a good place to start. Increase to 3+ times per week as long as you feel like you are recovering well.
- Type: Full-body resistance training is the cornerstone; add aerobic and balance work as tolerated.
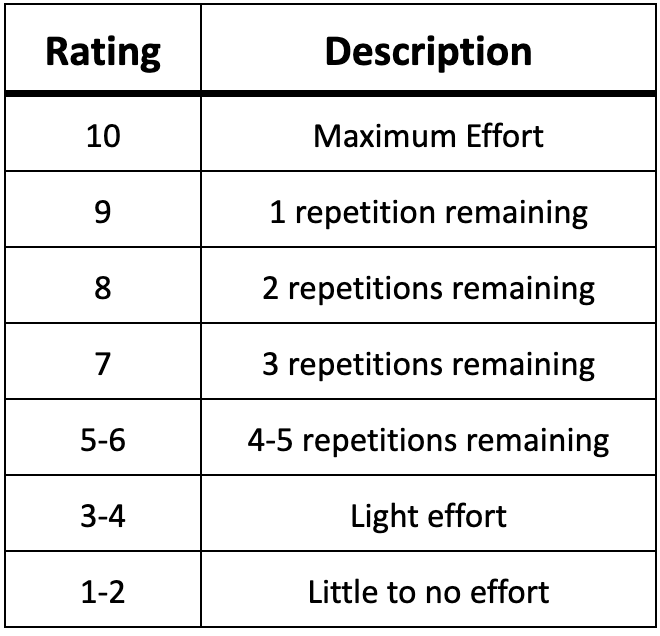
- Progression: Gradually increase intensity, duration, and volume. A helpful tool is the Repetitions in Reserve-Based Rating of Perceived Exertion Scale for Resistance Training (Table 1) [14], which allows you to rate the difficulty of a resistance training set based on how many more repetitions you believe you could have completed with maximum effort. Ultimately, your training should be challenging but doable. Focusing on performing as many repetitions as possible until you feel you have 2-5 “left in the tank” can be a good starting point.
Table 1. Repetitions in reserve-based rating of perceived exertion scale for resistance training. Adapted and modified from Zourdos et al., 2016 [14].
- Personalization: Tailor to individual needs, especially in those with injuries or comorbidities (e.g., diabetes, cancer, obesity). It’s ok if you can’t perform every exercise you may want to initially, and an experienced personal trainer can help you modify exercises to best fit your current capabilities.
Nutrition Guidelines:
- Protein Intake: 1.2–1.5 g/kg/day for older adults; including high-leucine foods.
- Distribution: Spread protein evenly across meals (≥25g/meal) to maximize muscle protein synthesis throughout the day.
- Supplements: Consider BCAA or protein supplements in older adults with low protein intake or appetite.
- Micronutrients: Ensure adequate vitamin D, C, and E for anti-inflammatory and anabolic support.
*Always check with your healthcare provider to ensure no contraindications to exercise or nutritional interventions before implementation*
Final Thoughts
Sarcopenia is part of the aging experience, but it’s a modifiable condition with proven interventions. All the things that give us strong muscles when we’re younger give us strong muscles when we’re older; strength just becomes gradually more challenging within that transition. Effective resistance training and adequate protein intake throughout our lifetime will set us up to weather that transition most successfully. Even if we feel like we’re “too late to the game,” we’re not – elderly adults engaging in resistance training for the first time still experience the benefits of improved strength, coordination, and balance – all of which foster greater independence and a higher quality of life. As always, consult with your healthcare providers to ensure no identifiable contraindications to exercise (e.g., injuries, unstable heart condition, myocarditis, uncontrolled metabolic disease, etc.) exist, and if you are cleared to exercise, engage in some form of resistance training that you enjoy. It can be lifting free weights, calisthenics (bodyweight exercises), weight machines, resistance bands, Pilates, or even a Shakeweight if we’re desperate – just do something to train the skill of physical strength. If you aren’t sure where to start, consider working with a health coach to help set clear goals and plans. Assuming no contraindications to exercise and that it is performed safely, resistance training is among the closest interventions to The Fountain of Youth.
While perhaps a bit intimidating, this information can be extremely liberating, as it highlights how minimizing the detriments of sarcopenia is within our control. There are currently no FDA-approved medications, which might very well change with advancing research on myostatins [15] in the coming years. Until then, the ever-growing aging population requires us to recognize sarcopenia not just as a condition of advanced aging, but as a condition whose burdens can be combatted through movement and nourishment.
If our goal is to maximize health and longevity, in which muscles and strength play critical roles, then prioritizing resistance training and protein intake is nonnegotiable.
- Salaffi, F., Carotti, M., Di Matteo, A., Ceccarelli, L., Farah, S., Villota-Eraso, C., Di Carlo, M., Giovagnoni, A. (2022). Ultrasound and magnetic resonance imaging as diagnostic tools for sarcopenia in immune-mediated rheumatic diseases (IMDRs). La Radiologia Medica, 127: 1277-1291. https://doi.org/10.1007/s11547-022-01560-y
- Cacciatore, S., Prokopidis, K., Schlögl, M. (2025). Osteoporosis and sarcopenia: two sides of the same coin. Euro Geriatric Med, In press. https://doi.org/10.1007/s41999-025-01275-z
- Goates, S., Du, K., Arensberg, M.B., Gaillard, T., Guralnik, J., Pereira, S.L. (2019). Economic impact of hospitalizations in US adults with sarcopenia. J Frailty & Aging, 8(2): 93-99. https://doi.org/10.14283/jfa.2019.10
- Shen, Y., Shi, Q., Nong, K., Li, S., Yue, J., Huang, J., Dong, B., Beauchamp, M., Hao, Q. (2023). Exercise for sarcopenia in older people: A systematic review and network meta-analysis. J Cachexia, Sarcopenia and Muscle, 14: 1199–1211. https://doi.org/10.1002/jcsm.13225
- Nasso, R., D’Errico, A., Motti, M.L., Masullo, M., Arcone, R. (2024). Dietary protein and physical exercise for the treatment of sarcopenia. Clinics and Practice, 14(4), 1451–1467. https://doi.org/10.3390/clinpract14040117
- Bohannon, R.W. (2019) Grip strength: an indispensable biomarker for older adults. Clin Interv Aging, 14: 1681–1691. https://doi.org/10.2147/CIA.S194543
- Nunes, E.A., Colenso-Semple, L., McKellar, S.R., Yau, T., Ali, M.U., Fitzpatrick-Lewis, D., Sherifali, D., Gaudichon, C., Tomé, D., Atherton, P.J., Robles, M.C., Naranjo-Modad, S., Braun, M., Landi, F., Phillips, S.M. (2022). Systematic review and meta-analysis of protein intake to support muscle mass and function in healthy adults. J Cachexia, Sarcopenia and Muscle, 13: 795–810. https://doi.org/10.1002/jcsm.12922
- Norton, L.E., Layman, D.K. (2006). Leucine regulates translation initiation of protein synthesis in skeletal muscle after exercise. J Nutrition, 136: 533S–537S. https://doi.org/10.1093/jn/136.2.533S
- Kramer, I.F., Verdijk, L.B., Hamer, H.M., Verlaan, S., Luiking, Y.C., Kouw, I.W.K., Senden, J.M., van Kranenburg, J., Gijsen, A.P., Bierau, J., Poeze, M., van Loon, L.J.C. (2017). Both basal and post-prandial muscle protein synthesis rates, following the ingestion of a leucine-enriched whey protein supplement, are not impaired in sarcopenic older males. Clinical Nutrition, 36: 1440–1449. https://doi.org/10.1016/j.clnu.2016.09.023
- Matthews, J.J., Arentson-Lantz, E.J., Moughan, P.J., Wolfe, R.R., Ferrando, A.A., Church, D.D. (2025). Understanding dietary protein quality: digestible indispensable amino acid scores and beyond. J Nutrition, In Press. https://doi.org/10.1016/j.tjnut.2025.07.005
- Volpi, E., Kobayashi, H., Sheffield–Moore, M., Mittendorfer, B., Wolfe, R.R. (2003).Essential amino acids are primarily responsible for the amino acid stimulation of muscle protein anabolism in healthy elderly adults. Am J Clin Nutr, 78: 250–258. https://doi.org/10.1093/ajcn/78.2.250
- Putra, C., Konow, N., Gage, M., York, C.G., Mangano, K.M. (2021). Protein source and muscle health in older adults: a literature review. Nutrients, 13(3): 743. https://doi.org/10.3390/nu13030743
- Fragala, M.S., Cadore, E.L., Dorgo, S., Izquierdo, M., Kraemer, W.J., Peterson, M.D., Ryan, E.D. (2019). Resistance training for older adults: Position statement from the National Strength and Conditioning Association. J Strength Cond Res, 33(8): 2019-2052. https://doi.org/10.1519/JSC.0000000000003230
- Zourdos, M.C., Klemp, A., Dolan, C., Quiles, J.M., Schau, K.A., Jo, E., Helms, E., Esgro, B., Duncan, S., Garcia Merino, S., Blanco, R. (2016). Novel resistance training-specific rating of perceived exertion scale measuring repetitions in reserve. J Strength Cond Res, 30: 267-275. https://doi.org/10.1519/JSC.0000000000001049
- Lee, S.J., Bhasin, S., Klickstein, L., Krishnan, V., Rooks, D. (2023). Challenges and future prospects of targeting myostatin/activin A signaling to treat diseases of muscle loss and metabolic dysfunction. J Gerontol Biol Sci Med Sci, 78(S1): S32-S37. https://doi.org/10.1093/gerona/glad033
- Johnson ML, Robinson MM, Nair KS. Skeletal muscle aging and the mitochondrion. Trends Endocrinol Metab. 2013;24(5):247-256. doi:10.1016/j.tem.2012.12.003 https://doi.org/10.1016/j.tem.2012.12.003
- Short KR, et al. Decline in skeletal muscle mitochondrial function with aging in humans. Proc Natl Acad Sci USA. 2005;102(15):5618-5623. doi:10.1073/pnas.0501559102
- Hepple RT, Rice CL. Innervation and neuromuscular control in ageing skeletal muscle. J Physiol. 2016;594(8):1965-1978. doi:10.1113/JP270561
- Basaria S. Reproductive aging in men. Endocrinol Metab Clin North Am. 2013 Jun;42(2):255-70. doi: 10.1016/j.ecl.2013.02.012. Epub 2013 Apr 6. PMID: 23702400.
- McPherron AC, et al. Regulation of skeletal muscle mass in mice by a new TGF-β superfamily member. Nature. 1997;387:83–90. doi:10.1038/387083a0
- Franceschi C, Campisi J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci. 2014;69 Suppl 1:S4–S9. doi:10.1093/gerona/glu057
- Buford TW, et al. Inflammation and aging: potential targets for intervention in sarcopenia. J Gerontol A Biol Sci Med Sci. 2010;65(5):478-486. doi:10.1093/gerona/glq029
- Breen L, Phillips SM. Skeletal muscle protein metabolism in the elderly: interventions to counteract the ‘anabolic resistance’ of ageing. Nutr Metab (Lond). 2011;8:68. doi:10.1186/1743-7075-8-68
- Sousa-Victor P, et al. Geriatric muscle stem cells switch reversible quiescence into senescence. Nature. 2014;506:316–321. doi:10.1038/nature13013
Related studies